Women are often told their fertility ‘falls off a cliff’ at 35, but is that right?
This article is republished from The Conversation under a Creative Commons license. Read the original article.

Karin Hammarberg, Monash University
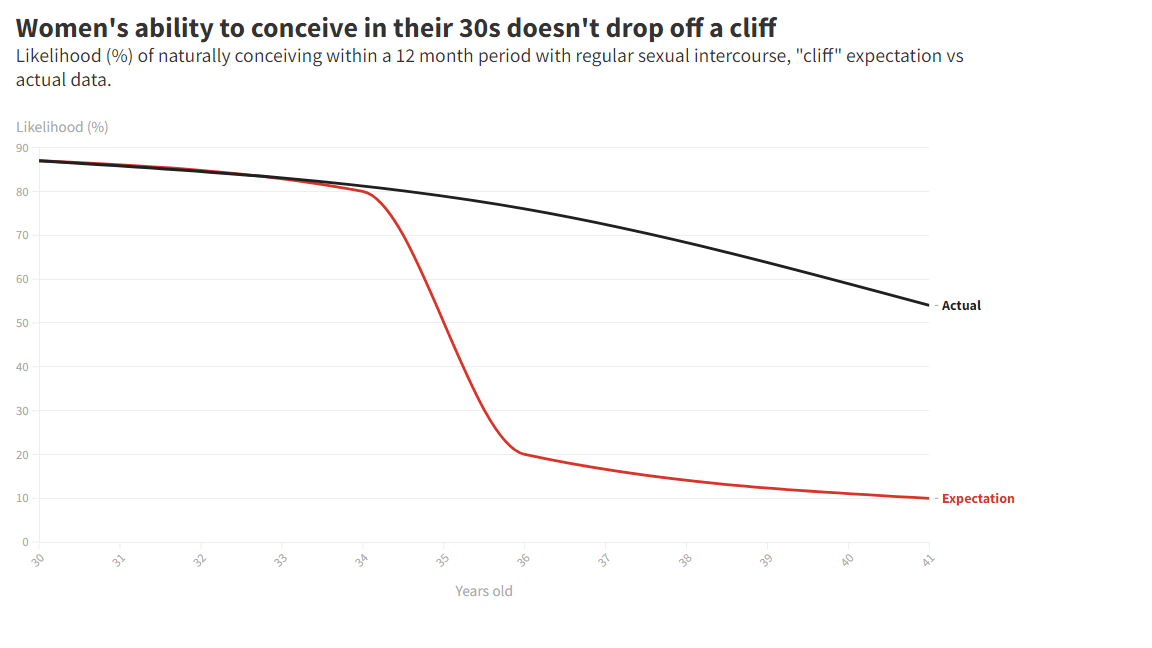
It’s a fact women’s fertility declines as they age. But the common description of fertility decline after age 35 as a “cliff” is more anxiety-provoking than factual.
If you want children, it’s important to understand the biology of fertility. This can help those who have a choice about timing to decide when to start trying for a baby.
And for those who don’t have a choice about timing, knowing what the options are can help make the best possible decisions.
Female ageing, egg numbers and quality
A baby girl is born with about one million eggs in her tiny ovaries, but by the time she reaches puberty there are only about 300,000 eggs left. This is a normal physiological process called atresia.
Of the eggs that remain when a woman starts having periods, only 300-400 will mature and be released in ovulation during the reproductive years. By the time a woman reaches menopause, there are no more functioning eggs in her ovaries.

While women in their mid- to late forties sometimes have “miracle babies”, the chance of pregnancy is minimal in the five to ten years leading up to menopause.
As women age, egg quality declines too. It’s estimated about 20% of all human eggs are “aneuploid”, which means they have the wrong number of chromosomes. This proportion increases as women age.
When an aneuploid egg is fertilised by a sperm it gives rise to an aneuploid embryo – which in most cases stops developing or ends in an early miscarriage.
What does this mean for the chance of a baby at different ages?
A woman’s most fertile years are between her late teens and late 20s. By around age 30, fertility starts to slowly decline and by mid-30s the decline speeds up.
But the decrease in chance of pregnancy after age 35 is gradual and more like a slope than a cliff, at least until age 40.
A large study that followed women trying for a baby found the chance of pregnancy after 12 months was 87% for women aged 30-31. This dropped to 76% at age 36-37, and 54% at age 40-41.
So up to age 41, most women who try for a baby will be pregnant after trying for up to 12 months. But the proportion who don’t achieve pregnancy increases with age, and the drop in chance is more noticeable after age 35.
Unfortunately, because the number of chromosomally abnormal (aneuploid) eggs increase with age, the risk of miscarriage increases as women age. For women in their early to mid-30s the risk of miscarriage is about one in ten. This increases to about one in three for women aged 40-44 years.
Source: Fertility and Sterility journal (actual data)
What about men’s age and fertility?
While it happens later in life than for women, men’s age affects the chance of pregnancy too. Sperm quality and fertility decline around age 45 and pregnancies fathered by men aged 45 or older are almost 50% more likely to miscarry than pregnancies fathered by men aged 25-29.
IVF is not a good plan B
Unfortunately, IVF can’t improve the quality of eggs, and the woman’s age is the biggest determinant of IVF success. Data from Victoria show that after three completed IVF cycles, 61% of women aged 34-35 when they started treatment had a baby.
The chance of a baby after three cycles at age 36-37 was 50% and at age 38-39 it was 38%. But by age 40-41 only 25% of women had a baby after three IVF cycles.
The chance of IVF success is also affected by the male partner’s age. Studies show that live-birth rates are lower in couples where the male partner is aged 45 or older than in couples where the male partner is younger than this.
What are the options?
Life circumstances, including not finding a partner who is willing to commit to parenthood, can prevent people from having children during their most fertile years.
Here are some options if you are worried about how age might affect your chance of having a baby:
-
going it alone: if you are single, you can consider joining the growing group of women who use donor sperm to become “solo mums by choice”. The safest option for you and your baby is to find a donor through a fertility clinic.
-
freezing eggs for later: while this might seem an attractive option, it’s costly and there is no guarantee of a baby down the track. To help you decide if this is the right option for you, here are some facts about egg freezing.
-
having IVF: if you are 35 years or older and have been trying for a baby for six months or more, see your GP for advice and basic fertility tests. Depending on test results, your GP can refer you to a fertility specialist. If you need IVF, sooner is better than later because age affects the chance of IVF success.
-
using donor eggs: the chance of a baby with IVF is negligible after age 40 unless you use eggs donated by a younger woman. Studies show after age 40, women using donor eggs are five times more likely to have a baby than women using their own eggs.
Finally, a word of caution. Ovarian reserve testing is often promoted as a way for women to find out their fertility and chance of getting pregnant.
The so called “egg timer” test measures the level of anti-mullerian hormone (AMH) in the blood, a hormone produced by reproductive tissues. The thinking is the more eggs present, the more AMH will be present, so it’s marketed as a type of “egg counting”.
However, research shows the test is not a reliable test of a woman’s fertility. On average, women of the same age have the same monthly chance of getting pregnant, regardless of their AMH level.
Karin Hammarberg, Senior Research Fellow, Global and Women's Health, School of Public Health & Preventive Medicine, Monash University