Fertility treatment explained
Understanding fertility treatment
There are many types of fertility treatments available, ranging from simple interventions such as medication to help a person ovulate, to more complicated procedures known as assisted reproductive treatment (ART). ART, also known as assisted reproductive technology, refers to medical and scientific methods used to help people conceive.
Fertility treatments can be used:
- to treat subfertility and infertility
- to help people who identify as LGBTQIA+, and single people have children
- for people who are unable to become pregnant, carry a pregnancy or give birth
- to reduce the chance of a child inheriting a genetic disease or abnormality
- to preserve fertility
When considering fertility tests and treatments, VARTA recommends asking the following five questions, designed by Choose Wisely Australia by NPS Medicine Wise:
- Do I really need this test, treatment or procedure?
- What are the risks?
- Are there simpler, safer options?
- What happens if I don’t do anything?
- What are the costs?
Additionally, VARTA recommends asking your doctor a sixth question:
- Will it improve my chance of having a baby?
Types of treatment
Depending on the cause of infertility, the following types of treatment may be recommended by your fertility specialist. This information provides a general overview of the techniques available. Speak to your fertility clinic for more information.
Ovulation induction (OI)
OI can be used if a person is not ovulating or not ovulating regularly. It involves taking hormone medication (tablets or injections) to stimulate follicle growth (the fluid-filled sacs where eggs develop). The response to the hormones can be monitored with ultrasounds and when the time is right, an injection is given to trigger ovulation (the release of the egg). Timing intercourse to coincide with ovulation provides the chance of pregnancy.
What are the benefits and risks of OI?
OI can be beneficial for people that have long, irregular, and infrequent menstrual cycles to help stimulate follicle growth and ovulation. However, the fertility medications used in OI that help stimulate follicle growth can cause multiple follicles to start developing. This means more than one egg may be released when you ovulate which increases the risk of multiple pregnancies. Your specialist may monitor your follicles developing on your ovaries via ultrasounds to ensure only 1 or 2 follicles grow. Another risk when using fertility medication is the risk of ovarian hyperstimulation (OHSS). OHSS can occur when the medications given cause your ovaries to produce a higher than normal number of follicles, which can lead to you becoming quite unwell. Symptoms include nausea, vomiting, diarrhea, shortness of breath, weight gain and dehydration. Although it is less likely to occur during OI cycles and more during in-vitro fertilisation (IVF) cycles, where higher doses of medications are given, it’s important to be aware of the potential risk. You can read more about OHSS here.
Artificial insemination (AI) or intrauterine insemination (IUI)
Artificial insemination, also known as IUI, involves the insertion of your partner or a donor’s sperm into the uterus of the person undergoing treatment at the time of or just before ovulation. IUI can be performed during a natural menstrual cycle, or in combination with hormone medications (tablets or injection). If a pregnancy is not achieved after a few rounds of IUI attempts, IVF with or without intracytoplasmic sperm injection (ICSI) may be needed. IUI can help those with irregular menstrual cycles or where the partner has minor sperm abnormalities. You can use the Unexplained infertility - exploring your options guide to better understand if IUI is a suitable option for you and discuss further with your clinic or fertility specialist.
The IUI process:
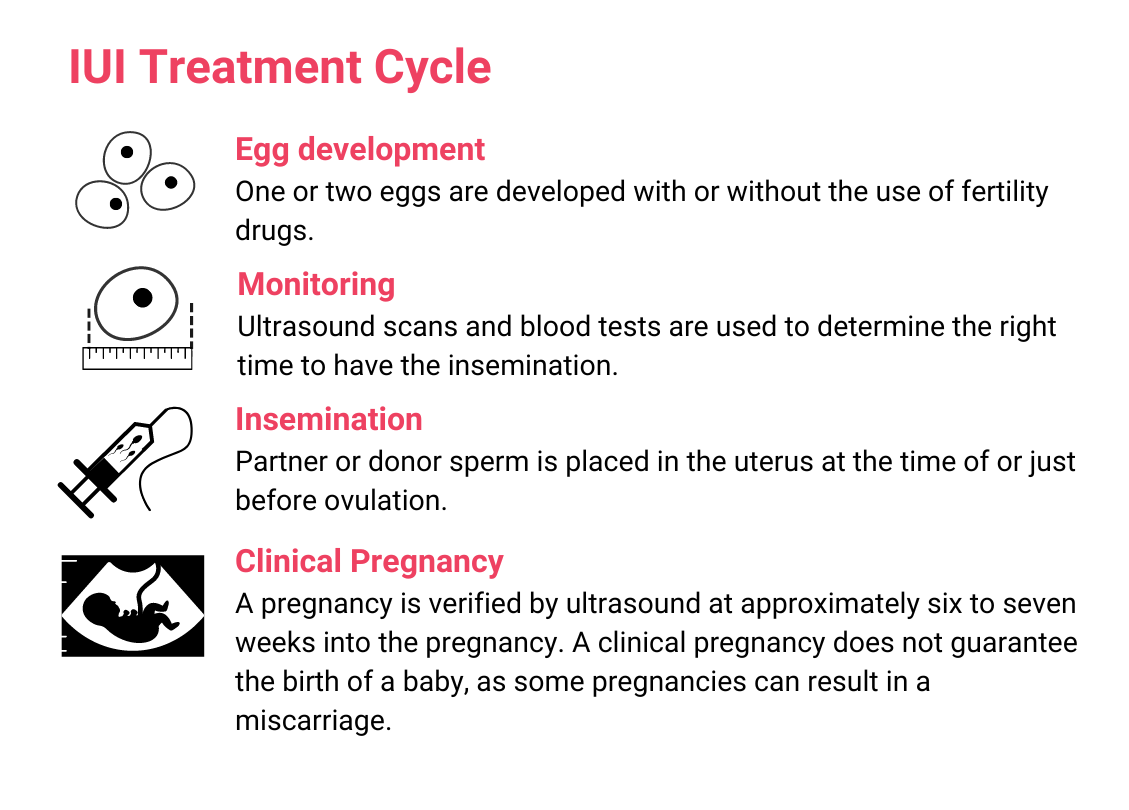
What are the benefits and risks of IUI?
IUI is a cost-effective non-invasive treatment compared to IVF. The most common risks associated with IUI are related to the medications that help stimulate follicle growth, as they can cause multiple follicles to start developing, meaning more than one egg may be released when you ovulate. This increases the risk of multiple pregnancies. Therefore, your specialist will monitor your follicles developing on your ovaries via ultrasounds and blood tests to ensure only 1 or 2 follicles grow for this procedure to proceed, and to minimise the risk. Another risk when using fertility medication is the risk of ovarian hyperstimulation (OHSS). OHSS can occur when the medications given cause your ovaries to produce a higher than normal number of follicles, which can lead to you becoming quite unwell. Symptoms include nausea, vomiting, diarrhea, shortness of breath, weight gain and dehydration. You can read more about OHSS here.
In-vitro fertilisation (IVF)
During your natural menstrual cycle, multiple follicles start growing. However, usually only 1 follicle is destined to ovulate and release an egg, as the rest go through cell death (atresia). During IVF, hormone injections are used to stimulate the ovaries to help enables multiple follicles to develop and be monitored and result in the multiple eggs being collected. When the developing follicles reach a certain size, indicating their potential of containing a mature egg (eggs ready to be fertilised with sperm), they are retrieved in an ultrasound-guided procedure under light anaesthetic. The eggs collected are placed with the sperm of your partner, or a donor in a culture dish in the laboratory to allow the eggs to hopefully fertilise, and embryos to develop. The embryos are monitored, and development is assessed over a period of time. Three to five days later, if suitable, one is placed into the uterus of the woman or person undergoing treatment in a procedure called an embryo transfer. If there is more than one embryo, the remaining embryo/s can be frozen and used in future treatment known as a frozen embryo transfer (FET).
The IVF process:
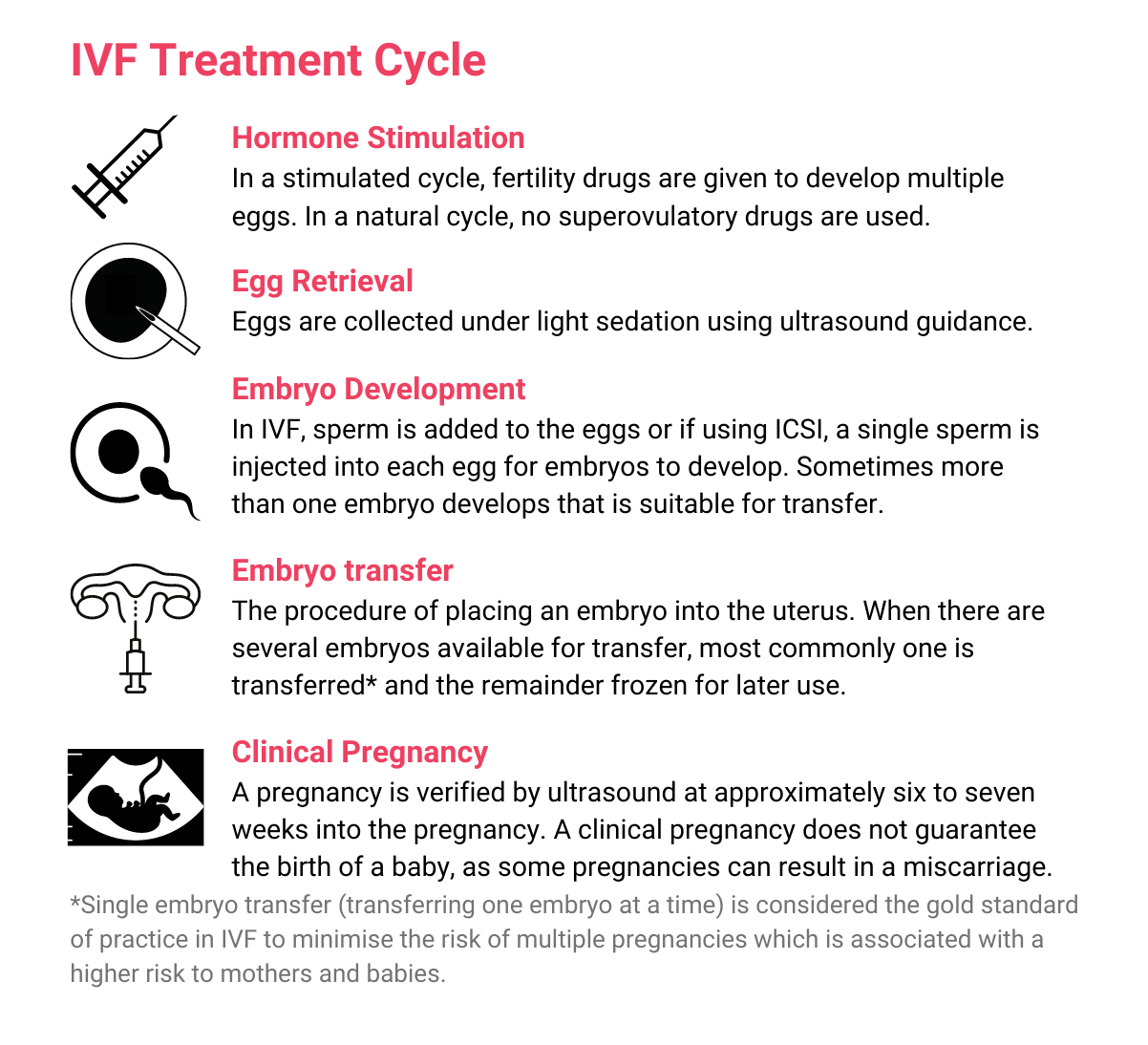
What are the benefits and risks of IVF?
IVF is a safe procedure and medical complications are rare. But as with all medical procedures, there are some possible health effects for both people undergoing treatment and for children born as a result of ART. Physical complications that need treatment in hospital occur in about one in 100 people going through stimulated IVF cycles. Examples include infection and bleeding post egg collection and OHSS. OHSS occurs as an excessive response to fertility medications taken during treatment to stimulate the ovaries to produce multiple eggs, which can be a potentially serious problem. IVF clinics monitor patients carefully to reduce the risk of OHSS. You can read more about OHSS here.
Research shows that IVF pregnancies are more likely to result in high blood pressure and diabetes later in pregnancy, deliver prematurely and give birth via caesarean section. About 6% of babies born from IVF have a birth anomaly, compared to about 4% of all other babies born via spontaneous conception. Although, the majority of birth anomalies are minor, most babies born after IVF are healthy and have no short or long-term problems. For more information, watch our webinar about what is known about the health of children and young adults born after IVF and ICSI here.
There are also individual factors that can increase your risk of pregnancy complications. Speak to your fertility specialist about your own circumstances and read more here about the possible health effects of IVF.
Understanding IVF success rates
Clinics report success rates in different ways, so when comparing clinics’ success rates make sure you compare like with like or ’apples with apples’. Most importantly, you need to consider your own personal circumstances and medical history when you estimate your chance of having a baby with IVF. You can read more about interpreting success rates here.
The chance of a live birth following IVF depends on many factors including the age of both people undergoing fertility treatment and the cause of infertility. Research using the Australian and New Zealand Assisted Reproduction Database calculated the chance of a woman or person undergoing treatment having a baby from their first cycle of IVF according to their age. The results below apply to people who used their own eggs, and it includes the use of frozen embryos produced by one cycle of IVF:
- Under 34 yrs: 44% chance of a live birth
- 35-39 yrs: 31% chance of a live birth
- 40-44 yrs: 11% chance of a live birth
- 44 yrs and above: 1% chance of a live birth.
Intracytoplasmic sperm injection (ICSI)
ICSI is sperm selection procedure used to overcome male factor infertility, which includes low sperm count, low sperm motility (movement), poor sperm morphology (shape) and problems with ejaculation. It may also be used in cycles involving frozen partner sperm, donor sperm, frozen eggs, or when no eggs become fertilised in a previous cycle with IVF.
ICSI follows the same process as IVF, except in ICSI the embryologist uses a microscope to select a single sperm that is injected into the egg to hopefully achieve fertilisation.
For couples with male factor infertility, research has shown ICSI is warranted to fertilise the eggs and give them a chance of having a baby. But for couples who don’t have male factor infertility, there is little evidence to demonstrate that using ICSI as the sperm selection technique in these circumstances increases the likelihood of a pregnancy.
What are the benefits and risks of ICSI?
ICSI has been proven to be beneficial and increase the chance of a live birth where male factor infertility has been diagnosed. Most babies born after IVF and ICSI are healthy and have no short or long-term problems. However, studies show that babies born following ICSI have a slightly higher risk of birth defects (6%) compared to babies conceived spontaneously (4%). There is a less than 2% chance that the egg can be damaged during the ICSI procedure.
Most pregnancies conceived by ICSI proceed without complications. Although, compared to spontaneous conceptions, both IVF and ICSI carry a small increase in the risk of still birth, premature birth, low birth weight and multiple birth. Studies show that the risk of miscarriage after ICSI is around 20% which is the same as after IVF.
What else do I need to know?
You can read more about what’s involved in ICSI and its possible health effects here.
Treatment "add-ons"
Fertility specialists are constantly looking for ways to improve your chance of getting pregnant through IVF or other fertility treatments. In the last few years an increasing number of ‘add-ons’, or ‘adjuvants’ have been offered by fertility clinics. They are tests, procedures or medications that are added to fertility treatment to try to improve the chance of success. But it’s important to know that many add-ons are experimental, have not been properly tested or have limitations to their studies, such as small sample sizes, risk of bias and insufficient data. So, it is not known if they make a difference to the chance of having a baby or if their use has potential risks.
Donor conception
There are many reasons why donor sperm, eggs or embryos may be needed.
Donor sperm
Donor insemination (DI) or IVF with donor sperm may be used when:
- a person does not produce any sperm
- a person does not produce normal sperm
- there is a high risk of a person passing on a genetic disease or abnormality to a child
- a person accessing treatment is a solo mum by choice, or
- a same-sex couple accessing treatment
The process of going through treatment via IUI or IVF with donor sperm is the same as outlined above.
If the woman or person going through treatment also has an infertility problem, donor eggs can be used in IVF treatment.
Donor eggs
Treatment with donor eggs may be needed when:
- a person doesn’t produce eggs, or their eggs are of low quality. This may be due to age or premature menopause (premature ovarian failure)
- there is a history of miscarriage/s, or
- there is a high risk of the person passing on a genetic disease or abnormality to a child
In these cases, hormone injections are used to stimulate the ovaries of the egg donor to produce the growth of multiple follicles and as a result, produce multiple eggs. When the developing follicles reach a certain size, indicating their potential of containing a mature egg (eggs ready to be fertilised with sperm), they are retrieved in an ultrasound-guided procedure under light anaesthetic. The donor’s eggs are then placed with sperm from the recipient's partner or a donor to fertilise, or if indicated, inseminated via ICSI. The embryos are monitored, and development is assessed over a period of time. Three to five days later, the embryo/s can either be frozen for future use or one can be transferred into the recipient’s uterus. This is known as a fresh embryo transfer. Be sure to speak to your clinic or fertility specialist to discuss your options and recommended treatment plan.
Donor embryos
Donor embryos can be used if a person or couple requires both donor sperm and donor eggs to achieve a pregnancy. Although rare, some people who have frozen embryos that they don’t intend to use, can choose to donate them for someone else to use.
In these cases, the recipient takes medications in preparation for the embryo transfer and when deemed ready, the embryo is thawed and transferred into the recipient’s uterus.
What else do I need to know?
You can find out more about donor conception here.
Surrogacy
Surrogacy involves a person with a uterus carrying a child for another person or couple with the intention of giving the child to that person or couple after birth. VARTA has some information and resources to assist people considering surrogacy. The Patient Review Panel, supported by administratively by the Victorian Government of Health staff, oversee approval for all surrogacy arrangements in Victoria.
You can find out more about surrogacy here.
Costs of ART treatments
In Australia, Medicare and private health insurers cover some of the costs associated with IVF but there are also substantial out-of-pocket costs.
Medicare also covers some of the costs associated with IUI procedures. This includes blood tests, ultrasounds scans, some treatment medications, sperm preparation and insemination procedures but there are also out-of-pocket costs associated with IUI treatment.
The difference between the Medicare contribution and the amount charged by the clinic is the ‘out-of-pocket cost’. These costs vary, depending on the treatment, the fertility clinic and whether you have reached the Medicare Safety Net threshold. You can read more about costs of treatment here.
For OI, ICSI, PGT and procedures with donor gametes (eggs, sperm or embryos) costs vary between each clinic and depend on the treatment plan and medications prescribed. For more information regarding costs it’s best to speak to your fertility clinic.
Helpful resources & support
Possible health effects of IVF
Understanding IVF success rates
ICSI and its possible health effects
Preimplantation genetic testing explained
The pros and cons of preimplantation genetic testing of aneuploidy (PGT-A)
Personal stories
Frequently Asked Questions
Where can I find out more about my fertility treatment options?
It’s helpful to know your options so you can make well-informed decisions. Talk to your fertility specialist and nurses about what to expect as part of your treatment and for resources about your treatment.
When should I seek the advice of a fertility specialist?
Speak to your GP about referral to a fertility specialist if you have been trying to get pregnant for 12 months or more of unprotected sex without success. If you are 35 years or older, it is recommended to seek advice after six months of trying unsuccessfully.
If you’ve tried to get pregnant for a year or more, and there’s no explanation for your lack of success, you have unexplained infertility. A fertility specialist can advise you on the best options. You can find out more about unexplained infertility here.
What should I think about when choosing a fertility specialist and clinic?
Fertility treatment is physically and emotionally demanding, and depending on your needs it can be expensive, so it is important to find a clinic and doctor that’s right for you. You can ask your GP for advice about choosing a fertility specialist, but you can also do your own research before committing to a doctor and clinic. You can read more about choosing a fertility specialist and clinic here.
What questions should I ask my doctor when considering IVF?
It is important to understand the success rates with different treatment options. Here are some questions to ask to help you get a realistic idea of your chance of having a baby with IVF.
- Considering your circumstances and medical history, what chance of having a baby can you expect?
- what is the clinic’s chance of a baby per started stimulated treatment cycle?
- What is the clinic’s chance of success for women of your age?
- What proportion of women in your age-group have embryos available for freezing after a stimulated treatment cycle?
- What is the cumulative chance of having a baby for a woman of your age if she has three stimulated treatment cycles?
You can read more about Understanding IVF success rates here.
Does IVF affect the long term health of babies?
Studies over the years have shown that babies born after fertility treatment are more likely to be born prematurely and to weigh less at birth, and they have a slightly greater risk of birth defects.
However, by the time they become adults, research has shown that they are just healthy as other people. You can read more here
